For many, hot flashes are the hallmark symptom of menopause, affecting up to 75% of women during this transition. They can strike suddenly, leaving you flushed, sweaty, and uncomfortable for one to five minutes at a time.
It may come as a surprise, but hot flashes can last seven to ten years, for up to 80% of menopausal women—disrupting sleep, daily routines, and overall well-being.
Hot flashes may be a natural part of menopause, but at Coral, we believe they shouldn’t have the power to take over your life. With the right strategies, it’s possible to manage and even reduce their frequency and intensity. In this article, we’ll explore five science-backed lifestyle shifts that can help you stay cool, comfortable, and in control.
The science behind a hot flash, simplified
The hypothalamus is a key brain region that helps maintain the body’s internal stability, or homeostasis, even as the external environment changes. Much like a home thermostat, it monitors body temperature and triggers responses to keep it within a comfortable range. A healthy individual’s core body temperature remains between 36.5°C to 37.5°C (97.7°F to 99.5°C). Even small deviations from this narrow range can be dangerous, highlighting the importance of precise temperature regulation.
Estrogen, a key female sex hormone, plays an important role in regulating the hypothalamus and keeping the body’s internal “thermostat” steady. But when estrogen levels decline during menopause, this regulation is disrupted. The thermostat becomes more sensitive, causing the body to overreact to even slight changes in temperature, leading to the perception of heat. This results in the unnecessary activation of cooling mechanisms like sweating and blood vessel dilation (vasodilation) which brings more blood to the skin’s surface allowing it to dissipate as heat, contributing to a hot flash.
What could a hot flash include?
Hot flashes can include any number of the following sensations.
- Sudden warmth in the chest, neck, and face
- Flushed or discoloured skin
- Sweating (typically upper body)
- Chills or shivering
- Heart palpitations
- Anxiety or unease
- Clammy skin
5 Preventative Strategies to Beat the Heat
Dress smart
Dress in a way that supports your comfort and confidence.
- Choosing lightweight, breathable fabrics like cotton, linen, or silk allows air to circulate and helps absorb moisture—which may help keep you cooler throughout the day.
- Try to avoid materials like polyester, nylon, and satin, which can trap heat and add to your discomfort.
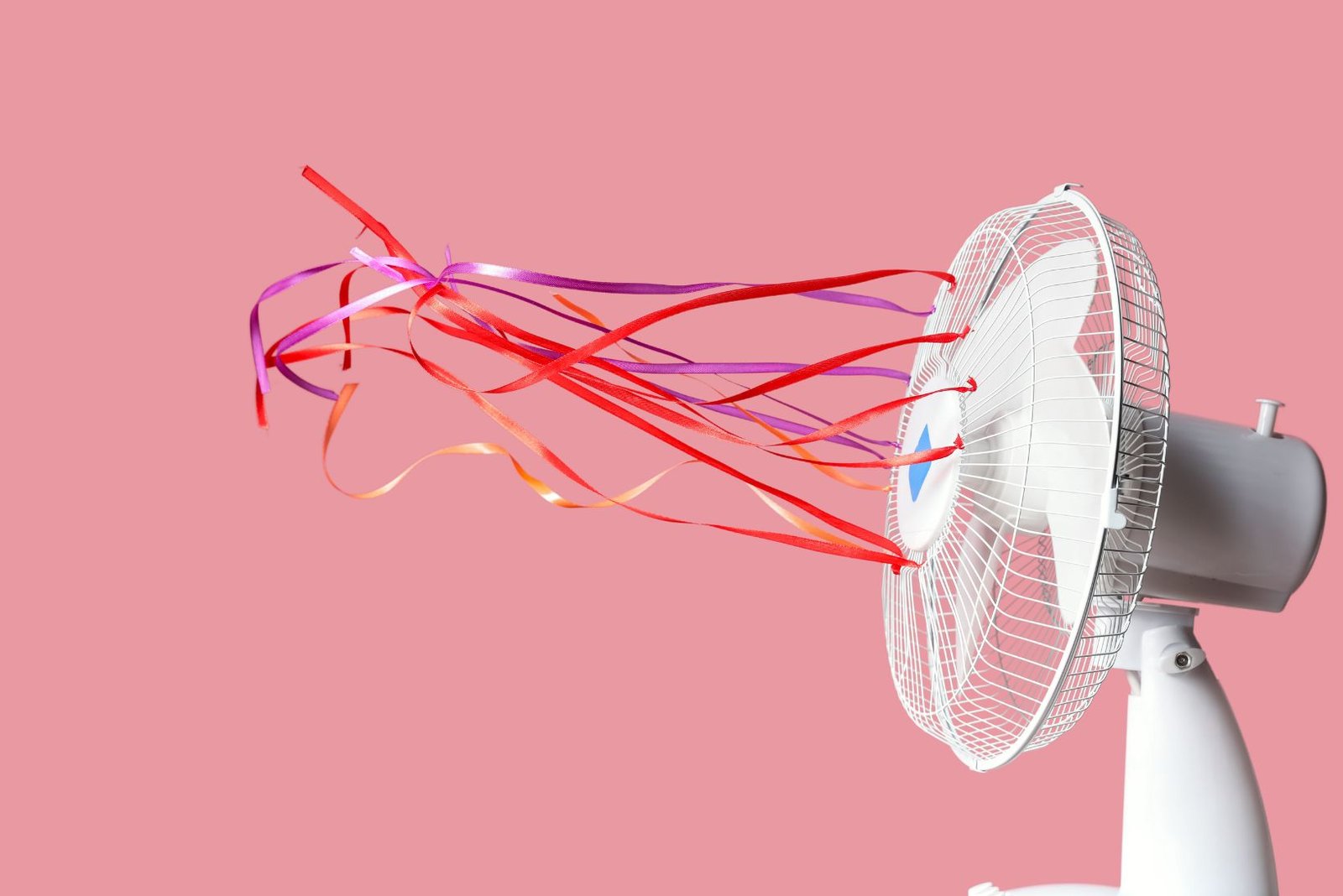
- It’s also helpful to have a portable cooling tool on hand. Whether it’s a handheld fan, a neck fan, a cooling blanket, or even cooling jewelry like bracelets and necklaces, these small supports can offer quick relief when you need it most on-the-go.
Sip smart
Support your body with simple, nourishing habits.
- Staying well-hydrated is key: drinking enough water helps replace fluids lost during hot flash-related sweating and keeps your body temperature more stable. Furthermore, regular water consumption protects against chronic disease by supporting various bodily functions, including kidney health, gastrointestinal function, and respiratory health during exercise.
- Be mindful of common triggers like caffeine, alcohol, sugar, and spicy foods, which can oftentimes intensify hot flashes.
- Although evidence is inconsistent across studies, herbal options such as soothing teas or supplements like soy or black cohosh—a plant from the buttercup family—may help relieve vasomotor symptoms like hot flashes for some individuals. These alternatives should be approached with caution, as effectiveness varies between individuals.
- Incorporating more fresh fruits and vegetables can be beneficial, as they consistently provide hydration, essential nutrients, support digestion, and aid the body’s natural detoxification processes.
Sleep smart
Night sweats, or hot flashes that strike during sleep, can leave you feeling restless and drained.7 But with a few thoughtful adjustments, you can create a more cooling and restful sleep environment.
- Try layering lightweight bedding that’s easy to remove or adjust throughout the night. If full-room cooling isn’t an option, some women find relief in placing a fan near their feet and lower legs to help regulate body temperature more effectively.
- Try sipping cool water 1–2 hours before bedtime to stay hydrated—just avoid drinking too much at once to minimize nighttime awakenings.
- As an alternative approach, studies have shown that cognitive behavioural therapy (CBT) can help reduce how bothersome hot flashes and night sweats feel by changing how you perceive and respond to them. Whether delivered in group sessions or through self-guided programs, CBT teaches individuals to recognize unhelpful beliefs—such as “I can’t cope with these hot flashes”—and reframe them into more constructive thoughts like, “This is uncomfortable, but it will pass.”
- It’s important to note that CBT does not eliminate hot flashes or night sweats. However, one particular study found significantly reduced symptom distress recorded by self-reported questionnaires at 6 and 26 weeks after implementing CBT. Particularly for women experiencing night sweats, CBT reduced sleep-related worry and rumination, which contributed to better sleep quality.
- CBT is a well-researched psychotherapy; however, like all treatments, it may not work for everyone and requires active engagement for best results.
Exercise smart
It’s well known that regular movement supports whole-body health—but for women navigating menopause, it can be especially powerful since a sedentary lifestyle can heighten the prevalence and severity of hot flashes.
- The majority of evidence from randomized control trials indicates that aerobic and resistance exercise training lead to a decrease in subjectively experienced hot flashes.
- Strength training could offer equally impressive benefits. In one small RCT study, postmenopausal women who followed a 15-week resistance program experienced nearly a 50% reduction in hot flashes. This effect is thought to be linked to an increase in β-endorphins—natural chemicals that not only enhance mood and relieve pain but also help regulate body temperature via the hypothalamus. This boost may help counteract the natural decline in β-endorphins seen after menopause.
- While ongoing research continues to explore how exercise impacts hot flashes across different women and life stages, the evidence is clear: movement is a powerful ally in managing global symptoms of menopause.
Relax smart
Stress is a well-known trigger for hot flashes and night sweats—but simple, intentional practices could help you make a real difference.
- Progressive Muscle Relaxation (PMR) is one such tool. By slowly tensing and relaxing each muscle group, the idea is to become more aware of the tension your body holds and how to release it. This technique has been shown to ease pain, reduce stress, and support better sleep.
- Beyond relaxation, PMR also strengthens the mind-muscle connection. Research shows that when you focus your attention on a specific muscle during movement, you can boost both its strength and muscle memory. In short, where your mind goes, your body follows.
Steps to Progressive Muscle Relaxation:
- Choose a quiet, distraction-free environment where you can comfortably settle and begin to relax.
- Starting from your toes and gradually progressing upward—through your calves, thighs, glutes, hands, arms, shoulders, abdominal muscles, face, and eyes—gently tense each muscle group for five seconds.
- Then, exhale slowly as you release the tension, allowing the muscles to relax for 10 to 20 seconds before moving on to the next group.
In addition to these 5 tips, many women benefit from tracking the frequency, severity, and triggers of their hot flashes. Identifying patterns can help you manage symptoms more effectively and evaluate how well treatments are working.
Hot flashes aren’t one-size-fits-all
Research has shown that timing, duration, and severity of hot flashes can vary among different ethnic groups. Indigenous and Black women have the most frequent and most bothersome hot flashes of all groups studied to date. Hispanic women experience hot flashes at similar rates to White women, but fewer than Black women. Chinese and Japanese women have the fewest hot flashes. If you find yourself comparing symptoms to women you know, pause and remember: every body is unique, complex, and beautifully its own. Relief isn’t one-size-fits-all—trust what your body is telling you, and adjust your care in ways that feel right for you.
Note: While hot flashes and night sweats are often linked to menopause, they can also stem from other medical conditions or medications. At Coral, our root-cause approach helps uncover what’s really going on—so your care plan is informed, intentional, and truly tailored to you.
Disclaimer: The information provided here is for informational purposes only. It is not intended as medical advice. Always consult with your doctor or healthcare provider to determine what is best for your individual health needs.
References:
- Hot flashes – symptoms and causes. Mayo Clinic. Published December 12, 2023. https://www.mayoclinic.org/diseases-conditions/hot-flashes/symptoms-causes/syc-20352790
- Hot Flashes | The Menopause Society. The Menopause Society. Published January 23, 2025. https://menopause.org/patient-education/menopause-topics/hot-flashes
- Osilla EV, Marsidi JL, Shumway KR, Sharma S. Physiology, temperature regulation. National Library of Medicine. Published 2023. https://www.ncbi.nlm.nih.gov/books/NBK507838/
- Charkoudian N, Stachenfeld N. Sex Hormone Effects on Autonomic Mechanisms of Thermoregulation in Humans. Autonomic Neuroscience. 2016;196(1):75-80. doi:https://doi.org/10.1016/j.autneu.2015.11.004
- Manz F, Wentz A. The Importance of Good Hydration for the Prevention of Chronic Diseases. Nutrition Reviews. 2005;63(1):S2-S5. doi:https://doi.org/10.1111/j.1753-4887.2005.tb00150.x
- Black Cohosh. NCCIH. Published May 2020. https://www.nccih.nih.gov/health/black-cohosh
- Clinic C. Hot Flashes: Triggers, How Long They Last & Treatments. Cleveland Clinic. Published March 31, 2017. https://my.clevelandclinic.org/health/symptoms/15223-hot-flashes
- Norton S, Chilcot J, Hunter MS. Cognitive-behavior therapy for menopausal symptoms (hot flushes and night sweats). Menopause. 2014;21(6):574-578. doi:https://doi.org/10.1097/gme.0000000000000095
- Witkowski S, Evard R, Rickson JJ, White Q, Sievert LL. Physical activity and exercise for hot flashes: trigger or treatment? Menopause. 2023;30(2):218. doi:https://doi.org/10.1097/GME.0000000000002107
- Berin E, Hammar M, Lindblom H, Lindh-Åstrand L, Rubér M, Spetz Holm AC. Resistance training for hot flushes in postmenopausal women: A randomised controlled trial. Maturitas. 2019;126:55-60. doi:https://doi.org/10.1016/j.maturitas.2019.05.005
- Aleem FA, McIntosh TK. Menopausal syndrome: Plasma levels of β-endorphin in post-menopausal women measured by a specific radioimmunoassay. Maturitas. 1985;7(4):329-334. doi:https://doi.org/10.1016/0378-5122(85)90056-8
- Mayo Clinic. Relaxation techniques: Try these steps to reduce stress. Mayo Clinic. Published January 24, 2024. https://www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/relaxation-technique/art-20045368
- Clark BC, Mahato NK, Nakazawa M, Law TD, Thomas JS. The power of the mind: the cortex as a critical determinant of muscle strength/weakness. Journal of Neurophysiology. 2014;112(12):3219-3226. doi:https://doi.org/10.1152/jn.00386.2014
- Gold EB, Colvin A, Avis N, et al. Longitudinal analysis of the association between vasomotor symptoms and race/ethnicity across the menopausal transition: study of women’s health across the nation. Am J Public Health. 2006;96(7):1226-1235. doi:10.2105/AJPH.2005.066936






